A new study from Indiana University School of Medicine’s Associate Research Professor Dr. Natalie Lambert finds that people who had COVID-19 could experience long-term symptoms not found on the Centers for Disease Control and Prevention website. These symptoms are referred to as “long-hauler” symptoms, and the group suffering from them are labeled as “longer-haulers”.
Dr. Lambert explains that most long-haulers who’ve had symptoms early on during their COVID infection — like shortness of breath — would never see those symptoms clear up completely. Other times, entirely new symptoms could appear, such as difficulty concentrating or severe nerve or joint pain.
“They realized that weeks, and sometimes months later, they just weren’t getting better,” Lambert said. “These are people who are simply not recovering in the time period that we expect.”
In collaboration with SurvivorCorps, a Facebook group and nonprofit organization that’s “dedicated towards organizing COVID-19 survivors in the fight against the virus,” Lambert posted a list of all of the COVID-19 long-term symptoms she thought were good contenders that people would have experienced the most.
Courtesy of SurvivorCorps Facebook
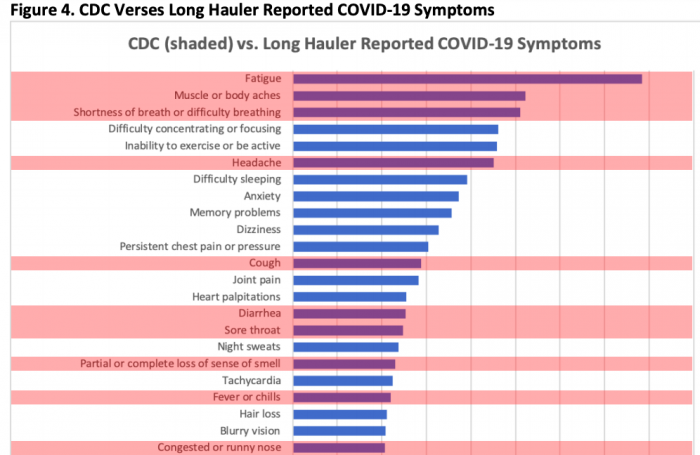
Then, she left the poll open for anyone within the group to add a symptom they were experiencing that wasn’t already listed. The CDC includes a list of 17 long-term symptoms. The participants in Lambert’s poll listed 98 new long-term symptoms not found on the CDC’s list.
“It was really an open-ended way of trying to understand what was the wide range of long-term symptoms that people were experiencing,” Lambert said.
These long-hauler symptoms in the Facebook poll included abdominal pain, confusion, night sweats, heart palpitations and memory problems.
Dr. Natalie Lambert speaks about several of the long-hauler symptoms.
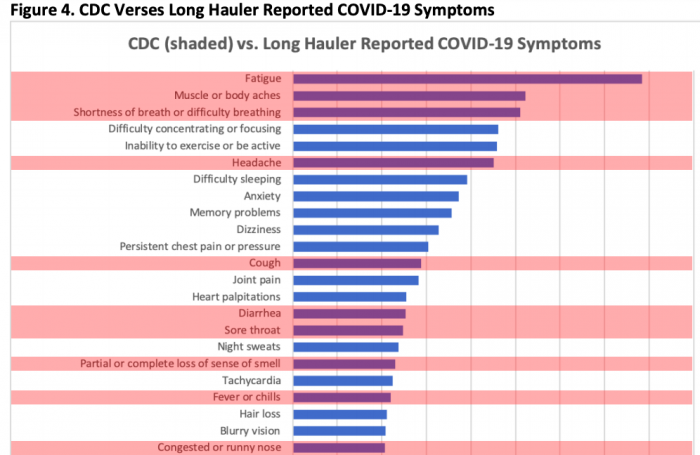
Courtesy of COVID-19 “Long Hauler” Symptoms Survey Report
The study shows that, “while the impact on the lungs and vascular system have received a lot of media attention, the survey suggests brain, whole body, eye and skin symptoms are frequent for those recovering from COVID-19.”
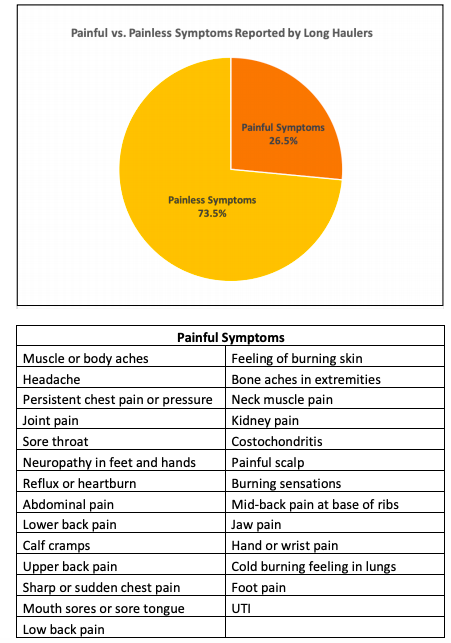
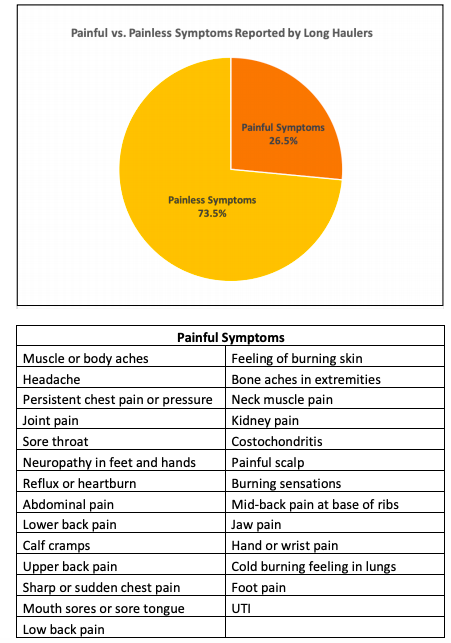
In addition, “a simple coding of the participant-reported symptoms according to which caused pain revealed that 26.5% of symptoms experienced by Long Haulers are painful.”
Though Lambert doesn’t know the exact number of responses — Indiana University School of Medicine doesn’t track individuals to protect their privacy — it was estimated there were between 1,400 and 1,500 responses.
Courtesy of COVID-19 “Long Hauler” Symptoms Survey Report
So, why are these symptoms not listed on the CDC website?
“A lot of the information you can find that’s talking about COVID is about the short-term symptoms,” Lambert said. “More research needs to be done on the long-term symptoms.”
This research includes treating this virus differently than other illnesses.
Lambert advocates for COVID-19 to not be treated like the yearly flu. By treating it as a virus that has both short and long-term effects, research and treatment can be targeted to specific symptoms before any more damage is done to the patient’s bodies.
“COVID is behaving really unexpectedly. It’s not behaving the way that a flu typically does,” Lambert said. “When a disease defies our expectations about what it’s supposed to be doing, it takes time for the medical community to kind of catch up to the new ways that things are happening.”
The lack of information about the broad range of COVID-19 symptoms “may and likely does drive people to unofficial sources of health information online,” according toLambert’s study.
Dr. Natalie Lambert explains what the next steps look like for long-haulers.
Currently, Lambert and her research team are using the results from the long-hauler study to conduct a more in-depth study that can hopefully predict the specific symptoms certain body types will experience if they are infected with COVID-19.
“Ultimately what we want to do is create predictive models that can help, such as, if you’re a male or female of a certain age, with underlying health conditions, here’s how we might predict COVID playing out for you,” Lambert said.
This survey took the approximate 4,000 participants several hours to complete. Questions asked about participants’ health history, the medications they were taking, demographic information and underlying health conditions.
They were also told to report when they got sick, when their symptoms arose, how severe these symptoms were, how it impacted their health and any treatments that helped them mitigate their symptoms.
Dr. Natalie Lambert explains her research team’s new follow-up study.